Third-degree and more severe burns damage both layers of the skin and may also damage the underlying bones, muscles, and tendons. Sometimes there is no pain because the nerve endings under the skin are destroyed. Third-degree burns have a high risk of infection. This surgery, done with general anesthesia, removes the injured skin and replaces it with healthy skin from an uninjured area of the body. Full thickness burns that are not grafted may take months or even years to heal.
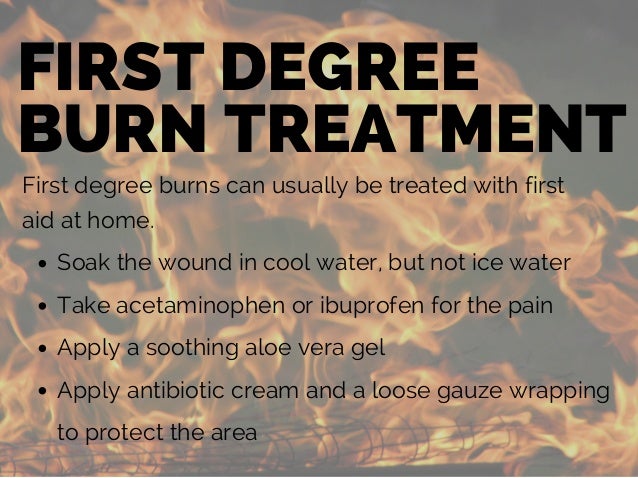
Burn survivors may have a combination of first, second, and third degree burns. Talk with your health care providers to better understand your specific injuries. Most burn injuries can be managed on an outpatient basis by primary care physicians. Prevention efforts can significantly lower the incidence of burns, especially in children. Burns should be managed in the same manner as any other trauma, including a primary and secondary survey. Superficial burns can be treated with topical application of lotions, honey, aloe vera, or antibiotic ointment.
Topical silver sulfadiazine is the standard treatment; however, newer occlusive dressings can provide faster healing and are often more cost-effective. Physicians must reevaluate patients frequently after a burn injury and be aware of the indications for referral to a burn specialist. When diagnosing a burn, a doctor evaluates the depth and extent of the damage, the degree of pain, the amount of swelling, and signs of infection. Doctors classify the burn based on the depth and extent of the injury.
In the emergency room, all wounds are wrapped with sterile cloths. People with burns are also evaluated for associated injuries . Doctors may also conduct tests to determine whether the wound is infected. The recovery and healing time of burns is dependent upon the severity of the individual burn. Third degree burns, the worst of the burns, do not heal in the same way as lesser burns, as they involve not only the skin but also layers of muscle and tissue beneath the skin. Treatment of burns depends directly on the causative agent and degree of injury.
Sunburns generally heal within two to five days and can be treated with aloe vera, low dose hydrocortisone creams, and pain medication. Other first and second-degree thermal burns should be immediately immersed in cool water for 10 or more minutes. In chemical burns the causative agent must be neutralized and removed as soon as possible. Restrictive items such as rings should be removed quickly before the area swells. Over the counter antibiotic ointments may be used. Small blisters should be left intact to heal, while large blisters may require medical removal.
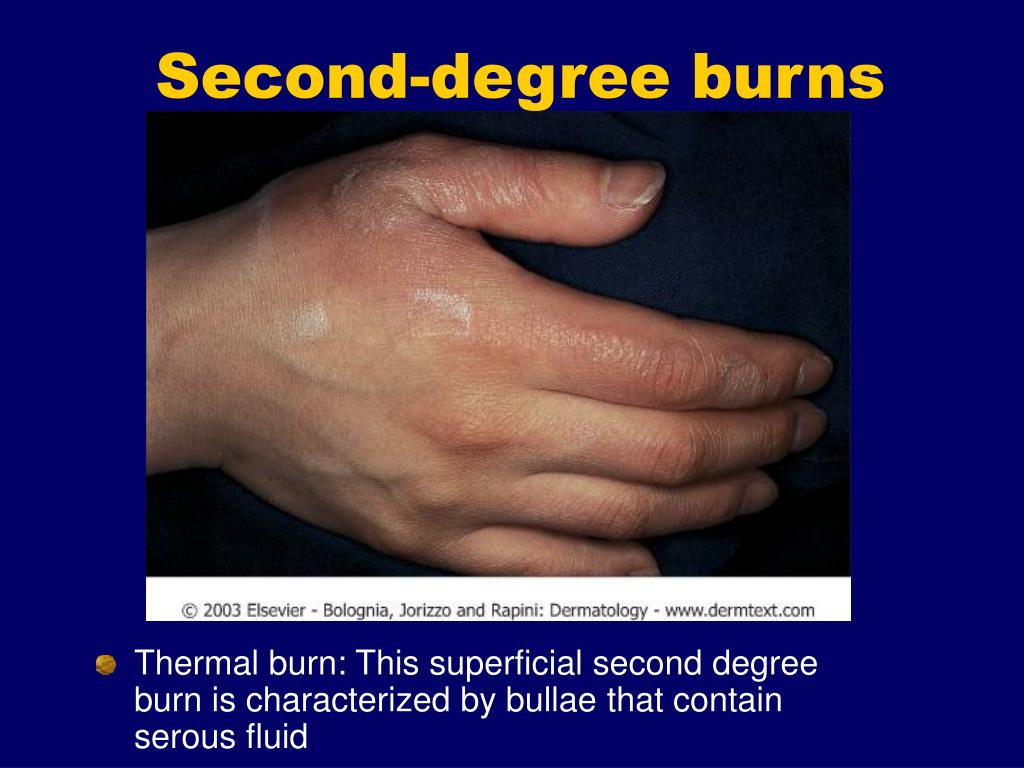
Deep partial thickness burns - these burns involve the epidermis and extend through most of the dermis. They are less red and are drier than superficial second degree burns. These burns may take up to a month to heal, and scarring may be extensive. Ice is not recommended as an initial treatment for burns because it can decrease circulation and make the burn worse.
Do not put any food-based products on the burn as this may cause infection and make it more difficult to clean the wound. Treat small burns with over-the-counter topical antibiotic ointment, like Polysporin or Neosporin, until healed. Burns heal better in a moist, covered environment. Third degree burns result in damage to all of the layers of the skin and require immediate medical attention. Simply clean the wound with cold water and cover the wound with a clean covering until you can reach the nearest emergency room. However, the treatment also depends on the size of the burn and its location.
First degree and smaller second degree burns are usually managed well at home. First aid may include soaking the burned area in clean cool water for a few minutes to stop the burning process, and then drying gently. Creams, such as aloe vera or burn ointments may help relieve some of the pain or discomfort. Keep the burns clean and loosely covered, and monitor for breaks in the skin and signs of infection.
Second degree burns can be extremely painful and create more serious skin damage as they include the epidermis and part of the underlying dermis. The burned area is red, swollen and blistered and may become infected if not properly cared for. These burns can often be treated with basic first aid but depending on their location or size may also require medical attention. Many people mistakenly apply ice to burns because it feels soothing, but ice can cause more harm than good in burn cases. Ice should not be applied to burns as it may cause nerve damage and frostbite, especially with more severe burns where the nerve may already be exposed. Using ice after the initial burn may slow the healing the process further and cause more damage to the surrounding skin.
Instead of ice, run cold water over the burn for several minutes following the initial burn. If you are unsure of first aid after a burn, it is always best to seek medical attention. All deep burns require treatment to prevent infection and scarring. Third-degree burns are the most serious type and can be life-threatening. However, first- and second-degree burns are more painful.
If you or a loved one has a blistering burn, prompt medical attention can aid healing. Talk to your healthcare provider about ways to lower your family's risk of accidental burns. First degree burns, often referred to as superficial burns, affect only the epidermis or outermost layer of skin.
When touched, skin that is burned superficially will blanch. The injured epidermis will slough off after a few days. These burns generally heal quickly and do not cause scarring. Antibiotic (an-ti-bahy-OT-ik) ointments or creams are often used to prevent or treat infections in patients with second-degree burns.
Using these ointments may require the use of bandages. Your doctor can assist you in coordinating the dressing changes with your pain medication. Dressings can be soaked off with water in a sink or shower. The skin and the burn wound should be washed gently with mild soap and rinsed well with tap water. Use a soft wash cloth or piece of gauze to gently remove old medications.
A small amount of bleeding is common with dressing changes. Your doctor will decide on the appropriate dressing and ointment. This will be based on the location of the burn, the need to control drainage, and your comfort. Second-degree burns go through the second layer of skin, called the dermis (DUR-mis). These burns cause pain, redness, and blisters and are often painful.
Surgery may be necessary for very deep second degree burns or those that are slow to heal. You can treat small 1st-degree burns on the hand yourself by holding the wound under cool water for 10 to 15 minutes. You should then cover the wound, using gauze and a loose bandage.
Do not apply ice, butter, egg whites or ointments, since these can worsen the injury and promote infection. If you're experiencing pain, consider taking an over-the-counter pain reliever, such as aspirin, naproxen, ibuprofen or acetaminophen. Do not give aspirin to children under two or to teenagers recovering from chickenpox or flu-like symptoms.
A bandage can be wrapped around the burn once ointment or cream is applied. When the first layer of skin has been burned through and the second layer of skin is also burned, the injury is termed a second-degree burn. Blisters develop and the skin takes on an intensely reddened, splotchy appearance. Second-degree burns produce severe pain and swelling.
If the second-degree burn is no larger than two to three inches in diameter, treat it as a minor burn. If the burned area is larger or if the burn is on the hands, feet, face, groin, buttocks, or is over a major joint, get medical help immediately. Second degree burns can be serious, especially if they cover a large area of the body. Most first-degree burns don't require medical attention, says Bernal.
She recommends rinsing the burn area with cool water for five to 10 minutes or until the pain subsides. Next, apply a moisturizing lotion and if needed, take an over-the-counter pain reliever for a few days. A burn is an injury to the skin resulting from direct contact or exposure from extreme heat or cold, friction, electricity, or chemicals. First-degree burns are superficial with red skin, pain, and no blistering. Second-degree burns involve destruction of the second layer of skin, causing blistering, swelling, and pain. Third-degree burns involve destruction of all layers of the skin, including fat, muscle, blood supply, and sometimes bone.
Third-degree burns do not have pain associated with them. Exposure to a dangerous acid or alkali can also cause skin damage that is referred to as a burn. There are several types of products the pharmacist can recommend for patients with first-degree or minor second-degree burns. Children under the age of 2 years who suffer burns should be checked by a physician.
Finally, burns of the hands, feet, face, and perineum should be referred. The hands may suffer severe functional problems with even minor burn scarring. Foot burns heal slowly and are prone to infection, and facial burns may be disfiguring.
It is difficult to apply dressings to the perineum, and the wound is easily irritated due to urine and fecal contact. Since some patients request help over the phone, it is prudent to request that they visit the pharmacy, so valuable visual input may be obtained. For example, the patient who denies blistering may have a first-degree or a third-degree burn, both of which would be immediately differentiated by a visual confirmation.
A prudent rule to follow in advising self-treatment is the color of the wound and the sensitivity, as these differ markedly in the superficial and deep second-degree burn. If there is any doubt as to severity, a physician referral is the wisest choice. Don't put ice or a cold pack on burned skin, as this can freeze the tissue and do even more damage. Run the injured area under lukewarm or slightly cool water for minutes. You may want to take an anti-inflammatory medicine like Advil or Tylenol to ease the pain and swelling. Make sure the burned area is no longer exposed to heat or burning materials, but do not attempt to remove any burned clothing .
Simply cover severe burns with a clean, moist cloth until examined by a doctor. Third-degree burns can be life threatening and always require skin grafts to heal. Even severe second-degree burns can cause serious harm. When in doubt, go to your local urgent care or an emergency room to have any burn evaluated.
First degree burns are typically superficial skin damages that do not exceed the top layer of skin. First degree burns can be painful but, in most cases, easily treated at home. They are often characterised by pain, redness, slight swelling and dryness but without blisters. Third degree burns are the ones we worry about because they are more likely to need a skin graft.
Any third degree burn should be seen in a burn center to see if it might heal with careful wound care or will require surgery. Burns are common personal injuries that can range considerably in severity. Burns are categorized into three degrees based on this severity, with third-degree burns being the most serious distinction that causes the greatest harm. Understanding the type of burn that occurred can help you determine the type of first aid to apply and the immediacy of help needed. Second-degree burns, or partial thickness burns, are more severe than first-degree burns.
They affect the outer layer of skin, called the epidermis, and part of the second layer of skin, called the dermis. If the burned skin or blisters have broken open, a bandage is needed. To further help prevent infection, apply a clean bandage whenever your bandage gets wet or soiled. If a bandage is stuck to a burn, soak it in warm water to make the bandage easier to remove. Be sure to read the product label for correct use.
The symptoms of a 2nd degree burn are similar to some of the symptoms of a 1st or 3rd degree burn. What makes it different is that the epidermis and dermis have been affected . A 2nd degree burn is caused in the same way that most 1st and 3rd degree burns are caused. The 2nd degree burn, however, is more serious than a mild burn and less serious than a severe burn.
Burns can happen in a variety of ways, but the most common causes are exposure to electricity, chemicals, sunburn, hot objects, boiling water, and fire. While some 2nd degree burns can be considered minor, they can also be very dangerous and sometimes life-threatening. Nobody enjoys the feeling of a sudden hot flash of pain against their skin. Even the most severe burns can happen in less than a second. How severe your burn is depends on what has scalded you and how long you were exposed to the cause of the burn. While you may be able to deal with a 1st degree burn on your own, a 2nd degree often requires professional medical attention.
Let's examine what makes a burn a 2nd degree burn. Hydrofibers, alginates and foam dressings may be used on superficial partial thickness burns. These products may require fewer dressing changes. In addition, they absorb exudate and keep the wound bed moist.